Clinical and Educational Supervision
All Clinical and Educational Supervisors have to be formally recognised, meeting the GMC standard and their status as a trainer has to be visible on their GMC registration status where it must say ‘This doctor is a trainer recognised by the GMC’ . Without this any training for a trainee will not count towards their CCT.
The framework for recognition is based on the seven areas that are deemed to form the basis of supervision [Academy of Medical Educators] and these are:
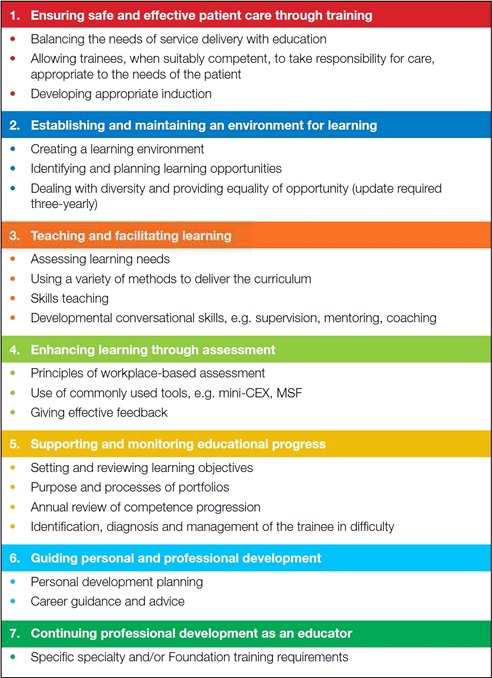
To be recognised or approved, trainers will need to meet the standards, as mapped against the seven areas. Educational Supervisors need to meet all seven standard areas while Clinical Supervisors should show evidence at appraisal that they have achieved and maintained competence in areas 1,2,3,4 and 7.
Provision of teaching and supervision to juniors and colleagues requires the expansion of competencies that most doctors have innately or have acquired in training. The use of those competencies for training can be developed progressively (teacher, mentor, Clinical Supervisor, Educational Supervisor, Training Program Director) using external provider courses, e-learning and feedback informed practice. Competencies are mapped against the seven framework areas outlined above, will become part of normal appraised practice and should lead to approval and registration as an educator with the GMC via the Deanery.
Training is a partnership between the supervisor and the supervisee. It requires the active involvement of both parties and within this partnership trainer and trainee both have responsibilities and obligations.
Clinical supervision relates to day-to-day oversight of trainees in the workplace and is an activity that involves all clinicians who come into contact with trainees.
The GMC (2012) defines a named Clinical Supervisor as ‘a trainer who is responsible for overseeing a specified trainee’s clinical work environment and is appropriately trained to do so. He or she will provide constructive feedback during the placement, and inform the decision about whether the trainee should progress to the next stage of their training at the end of that placement and/or series of placements.’
Educational supervision relates to the oversight of the trainees progress over time. Educational Supervisors are responsible for ensuring that trainees are making the necessary clinical and educational progress. Educational Supervisors will need all the skills of clinical supervision, plus an appreciation of supporting educational theory, the ability to undertake appraisal, work with portfolios and provide careers advice. Managing the trainee in difficulty will also involve the educational supervisor with support from training structures.
The GMC (2012) defines a named Educational Supervisor as ‘a trainer who is selected and appropriately trained to be responsible for the overall supervision and management of the trainees trajectory of learning and educational progress during a placement and/or series of placements. The educational supervisor’s role is to help the trainees to plan their training and achieve agreed learning outcomes. He or she is responsible for the educational agreement and for bringing together all relevant evidence to form a summative judgment at the end of the placements and/or series of placements.’
Mandatory training requirements for supervisors
It is recognised that supervisors will choose to access training from a variety of sources e.g. Royal Colleges, FOM, e-learning. Regardless of how, when or where training is undertaken it is expected that the seven areas of the professional development framework for supervisors will be covered.
Once undertaken, it is not necessary to repeat this training, although named Educational and named Clinical Supervisors are expected to demonstrate an ongoing commitment to their development as a medical educator through participation in a 3 yearly cycle of review.
The GMC (2012) states that ‘doctors can be named educational supervisor or named clinical supervisor without actively performing those roles all of the time. They must, though, maintain their skills by continuing to reflect on those roles – for example, through continuing professional development. This will need to be confirmed through their appraisal.’
All named Educational and Clinical Supervisors are expected to refresh their training in equal opportunities and diversity every three years.
This guidance has been produced to assist current and developing educators to achieve and demonstrate compliance with the Academy of Medical Educators seven areas of professional development.
| Clinical Supervisor | Educational Supervisor | ||
| 1 | Ensuring safe and effective patient care through training | X | X |
| 2 | Establishing and maintaining an environment for learning | X | X |
| 3 | Teaching and facilitating learning | X | X |
| 4 | Enhancing learning through assessment | X | X |
| 5 | Supporting and monitoring educational progress | X | |
| 6 | Guiding personal and professional development | X | |
| 7 | Continuing professional development as an educator |
X | X |
1. However, clinicians normally develop their interest in teaching and this must be reflected in a practical pathway. Summary of progression as an educator and professional development requirements:
| X=essential (X)=desirable |
Colleague Feedback | Intro to Med Ed | Med Ed Sup Cse | E-Learning | Postgraduate Certificate in Med Ed | PG Diploma and Masters in Med Ed |
| Teaching | X | (X) | ||||
| Mentor | X | X | ||||
| Clinical Supervisor | X | X | (X) | X | ||
| Educational Supervisor | X | X | X | X | (X) | |
| Trg Prog Dir | X | X | X | X | X | X – Dip (X) – MMEd |
2. The success of these activities is to be measured by the individual and senior colleague (Ed Sup or TPD) and can be summarised for use in the annual medical appraisal.
Initial Training
3. To become a named Clinical or Educational Supervisor initial training in the seven areas should be undertaken and evidence submitted to the local Deanery.
4. Summarise any relevant training (e.g. short courses, e-learning) undertaken in relation to your supervisory role and the Professional Development Framework area(s) to which it relates. Training may relate to more than one area.
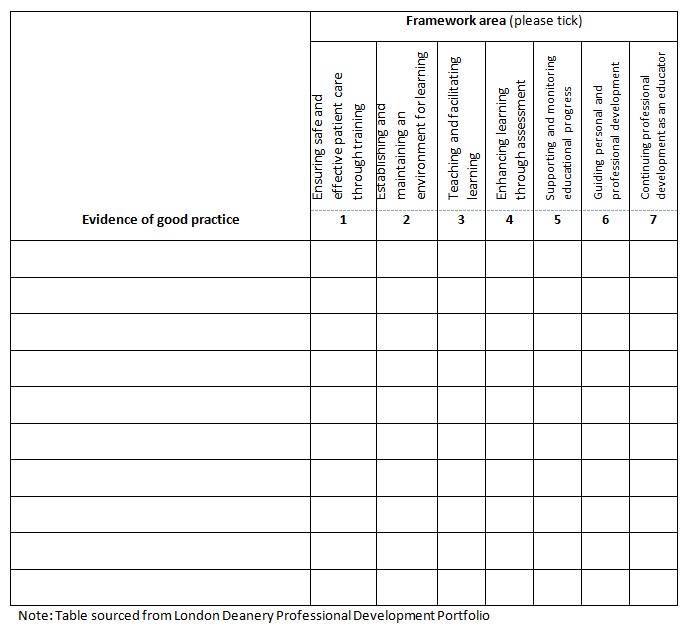 Download a handy Microsoft Word version of this table.
Download a handy Microsoft Word version of this table.
Review of Competencies
5. At least once during a revalidation cycle, your appraisal should include a comprehensive review of your educator status. On other years, the appraisal of the teaching component of your practice can be appraised alongside the rest of your work.
6. List the evidence of good practice that is being submitted and the Professional Development Framework area(s) to which it relates. Evidence must have been collected within the revalidation cycle or three years preceding the review (whichever is the longer) and where possible should include data from the latest GMC trainee survey or equivalent where available. Each piece of evidence may relate to more than one area.
7. CPD activities should cover at least two areas each year and over the revalidation cycle all seven areas must be covered.
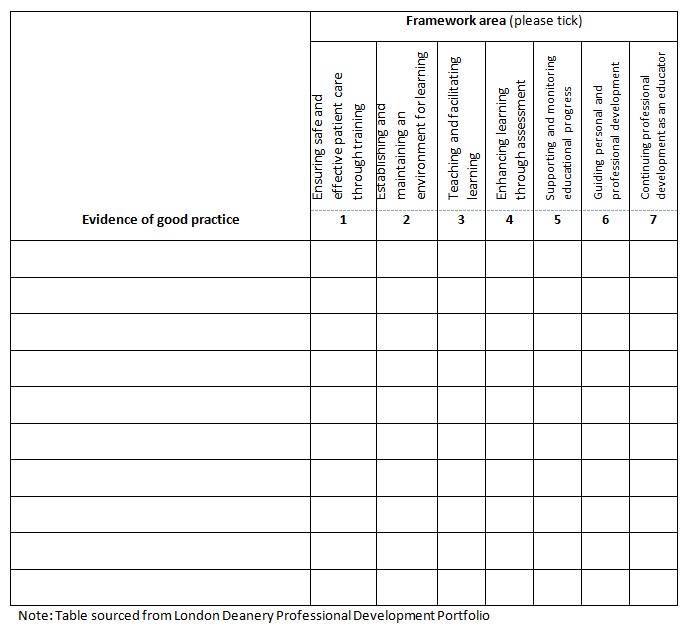 Download a handy Microsoft Word version of this table.
Download a handy Microsoft Word version of this table.
Examples of Evidence
| Area of professional development | Examples of evidence |
| 1. Ensuring safe and effective patient care through training |
|
| 2. Establishing and maintaining an environment for learning |
|
| 3. Teaching and facilitating learning |
|
| 4. Enhancing learning through assessment |
|
| 5. Supporting and monitoring educational progress |
|
| 6. Guiding personal and professional development |
|
| 7. Continuing professional development as an educator |
|
Note: Table sourced from London Deanery Professional Development Portfolio
Resources
- AoME: http://www.medicaleducators.org
- GMC: http://www.gmc-uk.org/education/10264.asp
- RCP London: http://www.rcplondon.ac.uk/cpd/non-clinical-cpd/supervision-and-appraisal/educational-supervisor-workshop-and-accreditation
- Oxford Deanery: http://www.oxforddeanery.nhs.uk/educator_development/educator_training.aspx
- Wessex Deanery: http://www.wessexdeanery.nhs.uk/courses__conferences_centre/educator-training_development/educational_supervisor.aspx
- Scotland: https://www.scotlanddeanery.nhs.scot/trainer-information/
- HEE: https://portal.e-lfh.org.uk/




