Approval of training programmes and posts
1.0 Introduction
The GMC has responsibility for the approval & re-approval of all postgraduate medical training programmes. All decisions on post and programme approval must therefore be made by GMC. This includes new posts and programmes (including ad personam/flexible programmes) applications for re-approval, where conditional approval was originally given.
The GMC considers training programmes and posts within their publication Promoting excellence: standards for medical education and training.
A learning environment should be safe for patients and supportive for learners and educators. The culture should be caring, compassionate and provide a good standard of care and experience for patients.
The learning environment and organisational culture should value and support education and training so that learners are able to demonstrate what is expected in Good Medical Practice and to achieve the learning outcomes required by their curriculum.
A generic medical training post should:
- deliver the curriculum and assessment requirements set out in the approved curriculum
- provide sufficient practical experience to achieve and maintain the clinical or medical competences (or both) required by their curriculum
- deliver an educational induction to make sure the learner understands the curriculum and how the post or clinical placement fits within the programme
- provide the opportunity to develop their clinical, medical and practical skills and generic professional capabilities through technology enhanced learning opportunities, with the support of trainers, before using skills in a clinical situation
- provide the opportunity to work and learn with other members of the team to support interprofessional multidisciplinary working
- ensure regular, useful meetings with clinical and educational supervisors
- deliver placements that are long enough to allow those in training to become members of the multidisciplinary team, and to allow other team members to make reliable judgements about their abilities, performance and progress
- have a balance between providing services and accessing educational and training opportunities. Services will focus on patient needs, but the work undertaken by doctors in training should support learning opportunities wherever possible.
- Education and training should not be compromised by the demands of regularly carrying out routine tasks or out-of-hours cover that do not support learning and have little educational or training value.
2.0 Overview
The duties, working hours and supervision of occupational medicine specialist trainees must be consistent with the delivery of high quality safe patient care. There must be clear procedures to address immediately any concerns about patient safety arising from the training of doctors.
Occupational Medicine training must be quality controlled locally by Deaneries, working with the Faculty, other stakeholders and training deliverers.
With regard to Equality, Diversity and Opportunity postgraduate training must be fair and based on principles of equality. Consideration of equality and diversity matters pervades the whole of the training – widening access and participation, fair recruitment, the provision of information, programme design and job adjustment. Responsibility to ensure that this is applied lies with the Postgraduate Deans and organisations providing training, trainers and trainees, other colleagues working with trainees, other stakeholders and the Faculty RSAs. Evidence of this comes from Surveys, outcome data, Deanery quality control data and visits.
All stages of training programmes must comply with employment law, the Equality Act, Equal Pay Acts, the Human Rights Act and other equal opportunity legislation that may be enacted in the future, and be working towards best practice. This will include compliance with any public duties to promote equality. Information about training programmes, their content and purpose must be publicly accessible either on or via links on Deanery and GMC websites. Deaneries must take all reasonable steps to ensure that programmes can be adjusted for trainees with well-founded individual reasons for being unable to work full- time to work flexibly within the requirements of GMC standards and rules. Deaneries must take appropriate action to encourage Trusts and other training providers to accept their fair share of doctors training flexibly. Appropriate reasonable adjustment must be made for trainees with disabilities, special educational or other needs.
Processes for recruitment, selection and appointment must be open, fair, and effective and those appointed must be inducted appropriately into training.
The requirements set out in the Faculty GMC approved curriculum must be delivered.
Trainees must be supported to acquire the necessary skills and experience through induction, effective educational supervision, an appropriate workload and time to learn.
Education and training must be planned and maintained through transparent processes which show who is responsible at each stage.
The educational facilities, infrastructure and leadership must be adequate to deliver the curriculum.
The impact of the standards must be tracked against trainee outcomes and clear linkages should be reflected in developing standards
The standards cover all postgraduate training programmes after the Foundation Years, for all specialties and to all places where postgraduate medical training is provided. This will include all occupational medicine training posts both within and outside the NHS. All training posts in occupational medicine will therefore need to meet these generic standards. The standards will be reviewed on a regular basis and the current version will be available on the GMC’s website.
The GMC will hold Postgraduate Deans responsible for meeting these standards across the UK and when making decisions on programme approval the GMC will take advice from Deaneries.
The GMC will normally approve training at the level of a programme, which is a series of posts (or rotation) that together enable a doctor undergoing training to acquire the competencies they need for the award of a Certificate of Completion of Training (CCT). Each post in a rotation must meet the generic standards. Where this is not the case, the problems will be addressed at post, programme or Deanery level, as appropriate. Posts within a single organisation are permissible, but it will need to be shown that all competences can be acquired within that post. Any more than 2 sessions per week at a location constitutes a post and so that location would need approval in its own right.
When the GMC approves a post or programme it does not set a time limit on that approval and approvals are therefore open ended.
3.0 Basic Requirements of a Training Programme in Occupational Medicine
A Training Post/Programme should provide a balanced and adequate range of instruction and experience in the principles of occupational medicine within a structured programme covering the GMC approved curriculum, with rotations and/or attachments as appropriate. In particular it will provide:
- a wide range of defined practical experience;
- increasing clinical and managerial responsibility with experience;
- protected training time during working hours to prepare for and undertake workplace based assessments and examination preparation;
- suitable and sufficient facilities to conduct a supervised dissertation project by research which is obligatory for the completion of training and award of MFOM;
The first year should be an introduction to occupational medicine and the functions of management and employee representatives in the workplace. The trainee should not be expected to spend more than 50% of their time in clinics.
The second year is concerned with enlarging experience and theoretical knowledge. The subject for research/dissertation should be chosen and work on the dissertation protocol started. An initial research proposal should be submitted and accepted by the Faculty before the end of ST4 (i.e. normally by the 24th month of full-time training in occupational medicine, or the part-time equivalent). It is therefore essential that trainees identify a suitable project and submit an initial proposal as early as possible in their training programme.
The third year consolidates the experience gained already and complements any deficiencies by secondments or visits to other industries and occupations.
In the final year, if not already achieved, individual responsibility should be taken for some aspect of the management of an occupational health service. The research project should continue and the dissertation.
4.0 Applications for Approval of a Training Post or Programme
- Applications for approval of a training post or programme in occupational medicine should be made by the educational supervisor(s) to the Regional Postgraduate Deanery who will then apply to the GMC using the application form which they access through GMC Connect.
- A training programme must be approved by GMC prior to recruitment of an StR. Time spent in a non-approved post cannot count toward training for CCT.
5.0 Programme Visits
Formal visits by the GMC will not normally be required for the approval of training posts.
5.1 GMC Triggered Visits
These visits are risk based, which means the GMC look at evidence and decide which areas of education are most likely to be of concern.
An outcome can be enhanced monitoring to support medical training organisations where there are concerns about the quality and safety of training.
In this circumstance the GMC will require more frequent progress updates from those responsible for managing these. They will be undertaken where possible serious educational failures which need urgent investigation occur and where concerns cannot be satisfied in any other way. They will not be used as a means of following up whether conditions attached to an approval have been met, which will be the role of the local Deanery. They are to investigate a concern or check on progress. The GMC publish information on enhanced monitoring cases on their website and share information with other healthcare regulators where appropriate.
Issues that require enhanced monitoring are those that could affect patient safety or training progression or quality. Issues are usually referred to the GMC if they meet the following criteria:
- Persistent and serious patient safety concerns
- Doctors in training’s safety is at risk
- Doctors in training are not getting the experience required
- Local quality management processes alone are insufficient to address the issue.
Concerns may be referred to the enhanced monitoring process by deaneries, local education and training boards, and royal colleges and faculties. The GMC can also escalate a concern to this process as a result of their own evidence or information from other sources (like patients and doctors in training).
Where possible they work with all organisations to address the concern and develop a sustainable solution. Sometimes there is a need to work with other regulators and organisations to make improvements. When local processes fail to address serious concerns, there may be use of legal powers to place conditions on the approval of postgraduate training posts. Conditions may be attached to any approval that have already been given. If it becomes clear that it is unlikely the conditions will be met, then approval for training may be withdrawn.
6.0. Quality Assurance
The responsibility lies with the Deanery and the GMC.
Annex 1
Occupational Medicine Training Post Checklist for Visitors, educational Supervisors and RSAs
This aide memoire should be read in conjunction with the post application details.
Organisation of the Post
- Check title
- Check code number
- Full or part time (If part time, record number of sessions)
- Company/organisation (If several, record details.)
- Site(s) (If several, record details and distribution of time between each.)
- To whom in the management structure does the trainee report?
(If appropriate, record for different companies and/or sites.) - With whom in the management structure does the trainee liaise on matters such as safety, welfare, environmental affairs?
(If appropriate, record for different companies and/or sites.) - What staff are responsible to the trainee?
(Record if different from shown on application.) - With whom does the trainee liaise externally on matters such as safety, welfare, environmental affairs, primary and secondary medical care of employees by others?
(If appropriate, record for different companies and/or sites.)
The Place or Places of Work
- Number of employees
- Type of work involved
- Main hazards
The Training Programme Director
(ie. Individual with overall responsibility for the Training Programme)
- Name
- MFOM/FFOM and on Specialist Register (Obligatory)
- Aware of duties and committed to undertaking them?
Clinical Supervisors
(Individual(s) who will provide day to day supervision during each stage/placement on the programme
– N.B. the educational and clinical supervisor may be the same person).
- Name(s)
- MFOM/FFOM and on Specialist Register (Obligatory)
- Aware of duties and committed to undertaking them?
- Do they work in same place as the trainee?
(If not, record place and access trainee has to him/her.)
Educational Supervisors
(Individual who will provide day to day educational supervision during each stage/placement on the programme – N.B. the educational and clinical supervisor may be the same individual).
- Names
- MFOM/FFOM and on Specialist Register (Obligatory)
- Aware of duties and committed to undertaking them?
- Do they work in same place as the trainee?
(If not, record place and access trainee has to him/her.) - Willing and able to oversee the education of the trainee on a daily basis and teach for half day per week during the first year, gradually reducing over the years to at least a minimum of half day each month in final year?
Opportunities for On-Job Training
- Does the post have opportunities for training across the curriculum?
Essential elements of training include:
- Surveillance of individuals or groups of workers at risk in a range of industrial technologies – What are the hazards, risks and specific medical problems? What surveillance is done, is it appropriate, and if so is its continued validity audited?
- Management of workers developing disease or injury in the course of their work – Is accident and emergency cover provided? Does the trainee have responsibility for first aiders and/or contribute to their instruction? Does he/she have involvement in long term management of chronic diseases and/or links with NHS, eg Clinical Assistant in “Chest Clinic”?
- Assessment of disability and fitness for work. Personal involvement in rehabilitation and assessment of workers – Are specialists in rehabilitation and/or physiotherapy employed on site and what are their links with the trainee? Is the trainee to visit rehabilitation and physiotherapy departments for instruction?
- Assessment and advice on various physical and psychological aspects of the working environment – What is done and by whom? Who initiates investigations? Is an occupational hygienist, ergonomist, occupational psychologist available and can the trainee gain instruction and experience from them?
- Involvement with all elements of industrial organisation including managers, educational supervisors, other employees, employees‟ representatives – What are daily links between the trainee and these people? What committees does the trainee sit on and in what capacity (executive or advisory)? What are management and union attitudes to medical services?
- Personal responsibility for the management of a department or some aspect of a department of occupational medicine, this responsibility to include aspects of audit and liaison with authorities responsible for environmental and community health – What are the responsibilities? What methods are used for clinical and business audit and what changes have been introduced as a result of audit?
Facilities
- Are the clinical facilities adequate?
- Is the secretarial assistance adequate?
- Is there adequate provision of textbooks, journals and other library services?
- Is there adequate information technology and instruction in its use?
The Training Programme
- Is there a definitive training programme detailing what the trainee will do in each of the years in post?
- Is the programme realistic?
- Does this programme make good use of the on-job training opportunities?
- Do you recommend any changes to make better use of these opportunities?
- Detail these changes.
- Does the programme provide adequate facilities and resources for the Workplace Based Assessments?
- Does the programme include adequate preparation for the end of Year 1 and final year examinations including where appropriate participation in an academic course?
- Is there sufficient study time allowed?
- Does the programme make good any deficiencies you identified in the on-job training opportunities by arrangements for visits and/or secondments to other industries or places of employment?
- Has the Educational Supervisor undertaken to act on the recommendations which you have told him and will be included in your report?
The Dissertation
- Have arrangements been made to select and progress a suitable investigation under appropriate supervision?
Annex 2
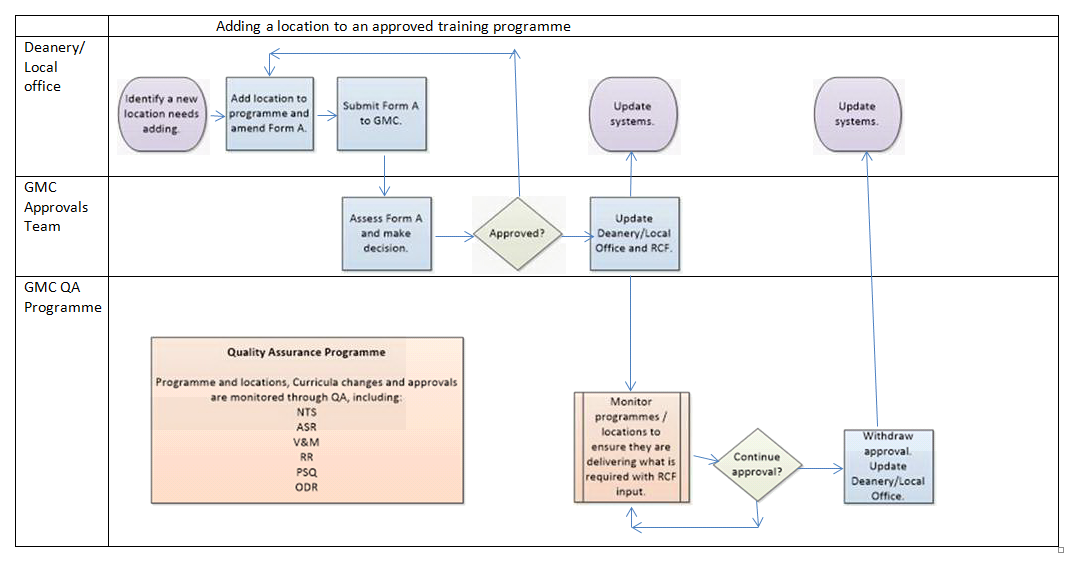
Process flow
(Click to expand)